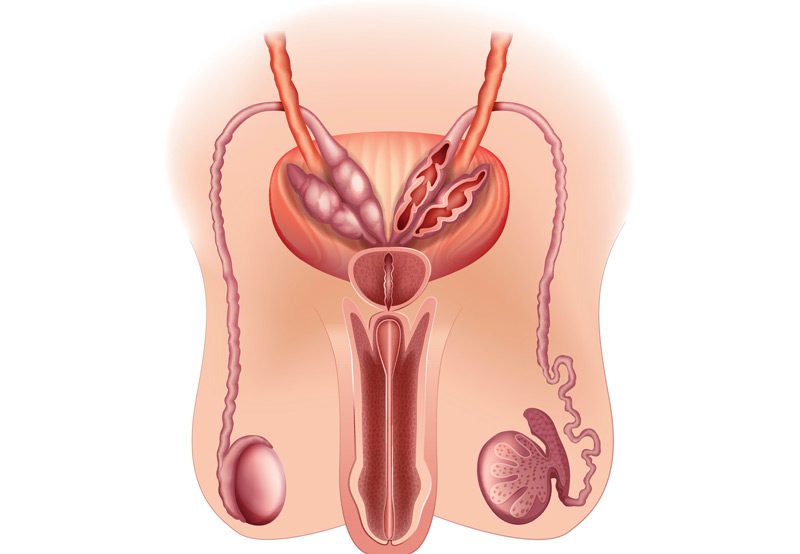

Testicular dysfunction refers to a variety of conditions that affect the function of the testes, leading to symptoms like low testosterone, infertility, and erectile dysfunction. The testes are responsible for producing sperm and testosterone, and any disruption in their function can have significant effects on male reproductive and sexual health. Symptoms may include low libido, difficulty achieving or maintaining an erection, changes in sexual performance, and infertility. These issues can be caused by a range of underlying conditions, including hormonal imbalances, infections, or injury to the testes.
Causes of Testicular Dysfunction
Testicular dysfunction can result from a variety of causes, including:
- Hormonal Imbalances: Low testosterone levels can impact sexual function, leading to reduced libido and erectile dysfunction.
- Genetic Conditions: Inherited conditions like Klinefelter syndrome or Y chromosome microdeletions can affect testicular function and fertility.
- Infections: Testicular infections, such as epididymitis or orchitis, can cause swelling and damage to the testes, impacting sperm production and hormone secretion.
- Trauma or Injury: Physical injury to the testes can cause long-term damage, affecting both sperm production and testosterone levels.
- Varicocele: An enlargement of the veins within the scrotum can lead to impaired sperm production and may affect testosterone levels.
- Chronic Health Conditions: Conditions like diabetes, high blood pressure, and obesity can negatively affect testicular function.
- Medications: Some medications, including chemotherapy, steroids, or certain antidepressants, can impair testicular function.

Diagnosis
To diagnose testicular dysfunction, healthcare providers may gather more information through:
- Medical History: Reviewing the patient’s health history, including any underlying conditions or medications that may affect testicular function.
- Physical Exam: Performing a physical examination to check for any signs of testicular injury, swelling, or abnormalities.
- Blood Tests: Measuring hormone levels, including testosterone, LH (luteinizing hormone), and FSH (follicle-stimulating hormone), to assess testicular function.
- Ultrasound: A scrotal ultrasound may be used to check for conditions like varicocele or structural abnormalities in the testes.
- Semen Analysis: A sperm count test can be performed to assess fertility and sperm quality.
- Genetic Testing: Genetic tests may be conducted if an inherited condition is suspected.
Treatment Options
Treatment for testicular dysfunction depends on the underlying cause and may include:
- Hormone Replacement Therapy: Testosterone replacement therapy (TRT) can help restore low testosterone levels, improving symptoms like reduced libido and erectile dysfunction.
- Surgery: Surgical correction of varicocele can improve sperm quality and testosterone levels in affected individuals. For men with testicular atrophy or who have lost a testicle, implants can be used for cosmetic purposes and to help restore hormonal balance.
- Lifestyle Modifications: Maintaining a healthy weight, regular exercise, and a balanced diet can improve overall hormonal health and sperm production. Quitting smoking can improve sperm quality and testosterone levels.
- Fertility Treatments: In cases of infertility, assisted reproductive technology options like sperm retrieval or in vitro fertilization (IVF) can assist in achieving pregnancy.
Next Steps
If you are experiencing symptoms of testicular dysfunction, it is important to consult with a doctor specializing in male reproductive and sexual health. Early diagnosis and treatment can help manage symptoms and improve overall health and fertility. With the right interventions, many individuals with testicular dysfunction can experience improvements in sexual function and quality of life.
