

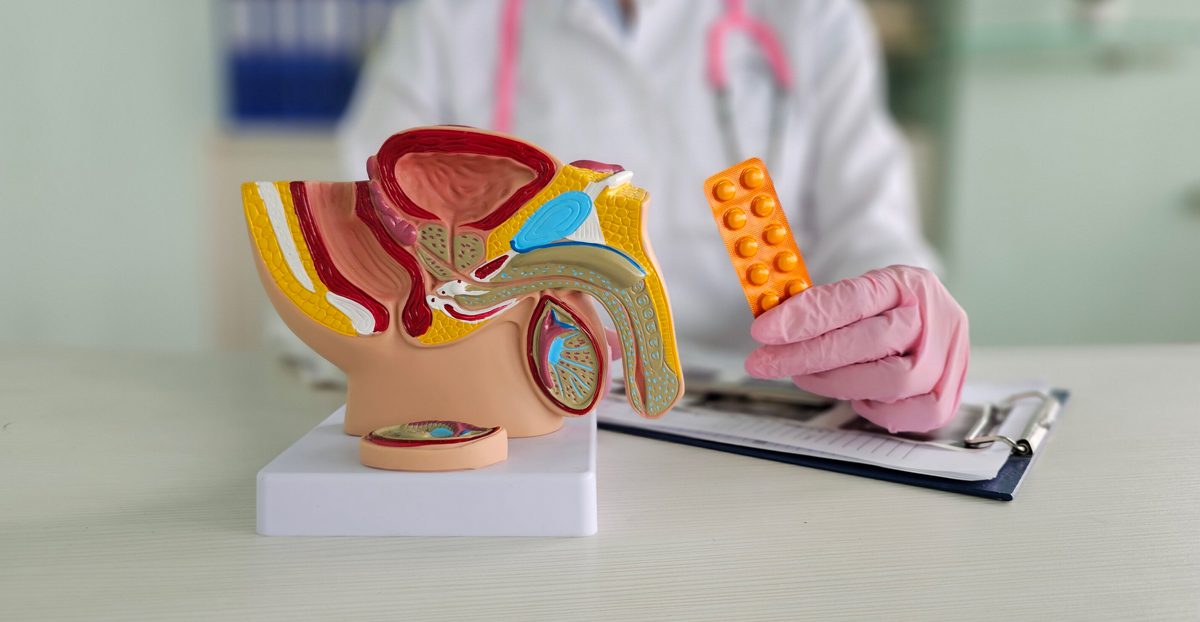
Male infertility refers to the inability to father a child due to issues with sperm production or function. Two primary conditions associated with male infertility are oligospermia (low sperm count) and azoospermia (no sperm in the ejaculate). Symptoms include difficulty conceiving, and in some cases, no additional signs of infertility may be present. Both conditions can be caused by factors related to sperm production, blockage, hormonal imbalances, or genetic conditions.
Causes of Male Infertility
Low sperm count, or the absence of sperm in the ejaculate, can be caused by factors such as hormonal imbalances, testicular damage, varicocele (enlarged veins in the scrotum), blockages in the reproductive tract, or lifestyle factors like smoking and excessive alcohol use.
Several factors can contribute to male infertility, including:
- Testicular Injury or Surgery: Any injury or surgery that affects the testicles can lead to sperm production issues.
- Genetic Conditions: Conditions like Klinefelter syndrome, Y chromosome deletions, or cystic fibrosis can affect sperm production.
- Hormonal Imbalances: Low levels of testosterone, high prolactin, or thyroid disorders can affect sperm production.
- Infections: Sexually transmitted infections (STIs), mumps, or other infections can affect sperm production or function.
- Lifestyle Factors: Excess weight can lead to hormonal imbalances that impair sperm production. Additionally, prolonged exposure to high temperatures, such as from hot tubs or working in hot environments, can reduce sperm count. Some medications, including chemotherapy and anabolic steroids, can lower sperm production.
Diagnosis
To diagnose male infertility, healthcare providers may utilize the following:
- Semen Analysis: A semen sample is analyzed to evaluate sperm count, motility, morphology, and overall quality.
- Blood Tests: Hormonal tests, including testosterone, FSH (follicle-stimulating hormone), and LH (luteinizing hormone), can help determine an underlying cause of infertility.
- Genetic Testing: Genetic tests may be performed to identify conditions like Klinefelter syndrome or Y chromosome deletions that could be affecting fertility.
- Scrotal Ultrasound: This test may be used to identify varicocele or other physical abnormalities affecting sperm production.
- Transrectal Ultrasound: This test helps evaluate the prostate and seminal vesicles, which can identify issues preventing sperm from reaching the ejaculate.
- Testicular Biopsy: In cases of azoospermia, a testicular biopsy may be conducted to check for blockages.
Treatment Options
Treatment for male infertility depends on the underlying cause and can include:
- Medications: If hormonal imbalances are identified, replacement therapy may help restore hormones to normal levels. If an infection is causing infertility, antibiotics can treat the infection and improve sperm production.
- Surgical Treatments: Surgery can repair a varicocele in the scrotum or address blockages in the spermatic ducts or epididymis, restoring the flow of sperm. Previous vasectomies may be able to be reversed.
- Lifestyle Changes: Depending on the cause of infertility, maintaining a healthy weight, regular physical activity, stopping smoking, and limiting alcohol can help to improve sperm function.
- Assisted Reproductive Technology (ART): In vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) may be used in cases where sperm count is low, with sperm being directly injected into the egg for fertilization. In cases of azoospermia, sperm may be retrieved directly from the testicles to use in fertilization.
- Sperm Extraction: Outpatient procedures to retrieve sperm may be utilized. With these procedures, sperm is cryopreserved for later use in IVF or ICSI.
These methods include:
- Micro-TESE (Microsurgical Testicular Sperm Extraction): Uses a high-powered microscope to locate and extract sperm from small, active areas of sperm production in men with non-obstructive azoospermia.
- TESA (Testicular Sperm Aspiration): Involves a small needle inserted into the testicle to aspirate sperm, often for men with obstructive azoospermia.
- PESA (Percutaneous Epididymal Sperm Aspiration): Involves aspiration of sperm from the epididymis, located behind the testicles. This is often utilized for men who have obstructive azoospermia following an infection or prior vasectomy.
Next Steps
If you suspect male infertility, it is important to seek an evaluation. Early diagnosis and treatment can significantly improve the chances of successful fertility outcomes. Depending on the cause of infertility, a variety of treatment options are available, ranging from lifestyle changes to advanced assisted reproductive techniques.
