
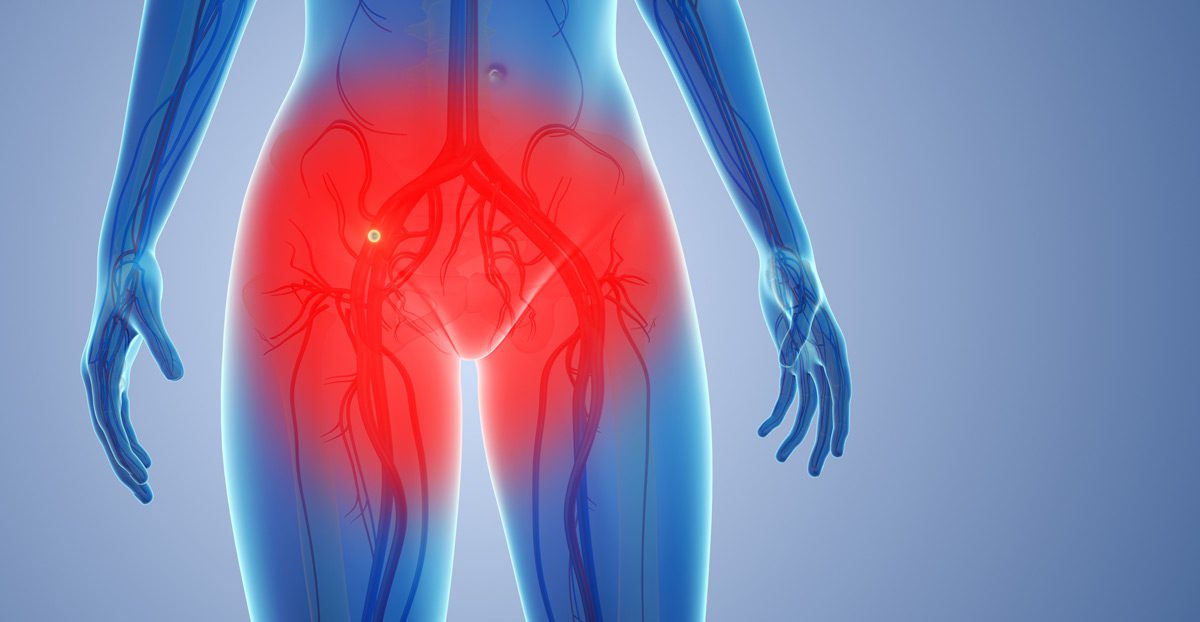
Pudendal neuralgia is a condition characterized by chronic pain in the pelvic region, specifically along the distribution of the pudendal nerve. The pudendal nerve provides sensation to the genitals, perineum, anus, and rectum. When this nerve becomes compressed, irritated, or damaged, it can lead to a variety of symptoms, including burning, stabbing, or aching pain. The pain may worsen with prolonged sitting, sexual activity, or certain physical activities.
Pudendal neuralgia is often associated with conditions such as childbirth, pelvic surgery, or trauma to the pelvic area. It can significantly affect quality of life due to its chronic nature and the impact it has on daily activities.
Causes of Pudendal Neuralgia
Pudendal neuralgia can be caused by:
- Childbirth: Vaginal delivery, particularly with prolonged labor, use of forceps, or large babies, can put pressure on or stretch the pudendal nerve.
- Pelvic Surgery: Surgeries such as hysterectomy, prostatectomy, or rectal surgeries can result in damage or compression to the pudendal nerve.
- Trauma or Injury: Pelvic trauma, including accidents or falls, may directly affect the pudendal nerve or surrounding structures.
- Chronic Sitting: Prolonged sitting on hard surfaces, especially in cyclists, can put pressure on the pudendal nerve and lead to irritation.
- Endometriosis: Tissue growth outside the uterus can affect the pelvic nerves, including the pudendal nerve.
- Anatomical Abnormalities: Abnormalities in the pelvic bones or ligaments may lead to increased pressure on the pudendal nerve.
- Nerve Entrapment: Compression of the pudendal nerve at various points in the pelvic area, such as at the level of the sacrospinous ligament, can result in pain.
Diagnosis
A healthcare provider may diagnose pudendal neuralgia through:
- Symptom History: A detailed discussion of pelvic pain, symptoms, and potential triggers, such as sitting or sexual activity.
- Physical Exam: A pelvic exam to assess tenderness in the pelvic region and rule out other causes of pain.
- Nerve Conduction Studies: Tests that measure the function of the pudendal nerve and assess for signs of nerve damage or dysfunction.
- MRI or CT Scan: Imaging to detect any anatomical abnormalities or compressive factors affecting the pudendal nerve.
- Electromyography (EMG): A test to evaluate muscle function and determine if the pudendal nerve is being affected.
- Pudendal Nerve Block: A diagnostic test in which an anesthetic is injected near the pudendal nerve to temporarily relieve pain, confirming the diagnosis of pudendal neuralgia.
Treatment Options
Treatment for pudendal neuralgia may include:
- Pain Management: Medications such as anti-inflammatory drugs and nerve pain medications (e.g., gabapentin) may be used to manage pain.
- Physical Therapy: Specialized pelvic floor physical therapy to reduce muscle tension and improve pelvic alignment, relieving pressure on the pudendal nerve.
- Nerve Blocks: Injection of local anesthetics or steroids around the pudendal nerve to reduce inflammation and provide temporary pain relief.
- Transcutaneous Electrical Nerve Stimulation (TENS): A therapy that uses electrical pulses to reduce pain and promote healing in the affected area.
- Lifestyle Changes: Avoiding prolonged sitting, using cushioned seats, and modifying daily activities to reduce pressure on the pudendal nerve.
- Surgical Decompression: In severe cases, surgery may be performed to relieve pressure on the pudendal nerve by removing the source of compression.
Next Steps
If you are experiencing pelvic pain, especially with activities like sitting, sexual activity, or bowel movements, consult with your doctor for an accurate diagnosis. Pudendal neuralgia is a complex condition that can be effectively managed with a combination of pain relief, physical therapy, and lifestyle adjustments. Early intervention can improve symptoms and help restore normal function.
