

Pelvic floor dysfunction occurs when the muscles of the pelvic floor, which support the bladder, uterus, rectum, and small intestine, become weakened, tight, or imbalanced. This can lead to a range of symptoms, including urinary incontinence, pelvic pain, constipation, and difficulty with sexual function. Pelvic floor dysfunction can result from various factors, including childbirth, aging, trauma, surgery, or chronic health conditions. The severity of symptoms can vary, but the condition can significantly impact quality of life if left untreated. Treatment typically involves a multi-disciplinary approach with pelvic floor specialists for physical therapy.
Causes of Pelvic Floor Dysfunction
Pelvic floor dysfunction can be caused by:
- Pregnancy and Childbirth: Vaginal delivery, particularly of larger babies or multiple pregnancies, can stretch or damage the pelvic floor muscles.
- Aging: As the body ages, pelvic floor muscles may lose strength and elasticity, leading to dysfunction.
- Chronic Straining: Conditions such as chronic constipation or heavy lifting can put prolonged pressure on the pelvic floor.
- Obesity: Excess weight can put additional strain on the pelvic floor muscles.
- Trauma or Surgery: Pelvic surgery, particularly for conditions such as hysterectomy, can damage the pelvic floor muscles and nerves.
- Neurological Conditions: Conditions like multiple sclerosis or spinal cord injuries can affect nerve function and impair pelvic floor muscle control.
Diagnosis
A healthcare provider may diagnose pelvic floor dysfunction through:
- Symptom History: A thorough discussion of symptoms such as pelvic pain, incontinence, constipation, or sexual dysfunction.
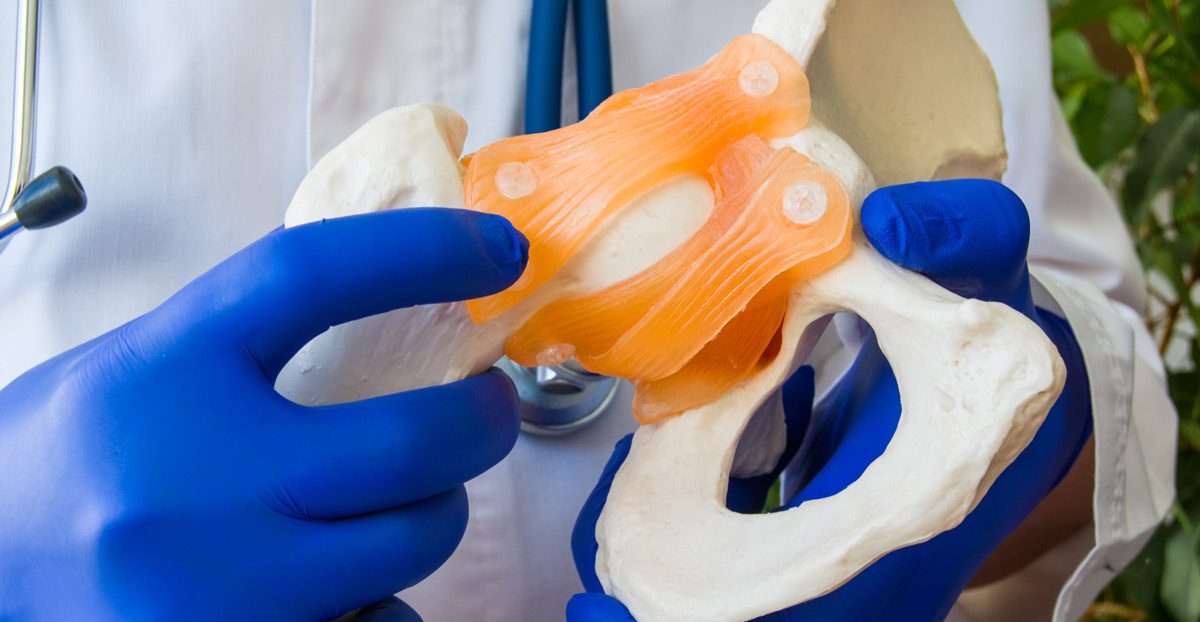
- Physical Exam: A pelvic exam to assess muscle tone, strength, and any abnormalities in the pelvic floor area.
- Urodynamic Testing: To evaluate bladder function and detect issues related to urine flow or retention.
- Imaging Tests: Ultrasound or MRI to assess the anatomy and structure of the pelvic floor.
- Pelvic Floor Muscle Biofeedback: A technique used to assess and retrain pelvic floor muscles by monitoring muscle activity during contractions.
Treatment Options
Treatment for pelvic floor dysfunction may include:
- Pelvic Floor Physical Therapy: Specialized exercises and techniques to strengthen, relax, or retrain the pelvic floor muscles.
- Biofeedback Therapy: A technique that uses sensors to provide real-time feedback on pelvic floor muscle activity, helping patients improve muscle control.
- Pelvic Floor Muscle Training (Kegel Exercises): Strengthening exercises that target the pelvic floor muscles to improve control and reduce symptoms of incontinence.
- Medications: Anticholinergic medications for overactive bladder or stool softeners for constipation.
- Vaginal Pessaries: A device inserted into the vagina to provide support to the pelvic organs and reduce prolapse or incontinence.
- Surgery: In severe cases, surgical options such as prolapse repair, sling procedures, or bladder neck suspension may be considered to correct pelvic floor issues.
- Pain Management: Medications or therapies for pelvic pain, including nerve blocks or trigger point injections, may be used to manage discomfort.
Next Steps
If you are experiencing symptoms of pelvic floor dysfunction, such as incontinence, pelvic pain, or difficulty with bowel movements, consult with your healthcare provider for a thorough evaluation. Early diagnosis and treatment can improve symptoms and strengthen pelvic floor muscles.
